[vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-bottom:0px; padding-bottom:0px;»][vc_column alignment=»left» width=»1/2″]
Statin
[/vc_column][vc_column width=»1/2″]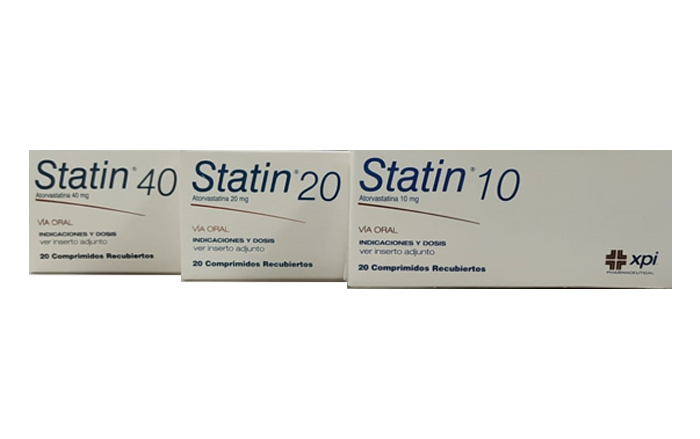 [/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]Description
Statin contains Atorvastatin Calcium, a synthetic lipid lowering agent, inhibitor of 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase. This enzyme catalyzes the conversion of HMG-CoA to mevalonate, an early and limiting step in cholesterol biosynthesis.
Clinical pharmacology
Mechanism of action: Atorvastatin is a selective and competitive inhibitor of HMG-CoA reductase, the limiting enzyme responsible for the conversion of 3-hydroxy-3-methyl-glutaryl-coenzyme A to mevalonate, a precursor of sterols, including cholesterol. Triglycerides and cholesterol in the liver are incorporated into VLDL and released in plasma to be carried to peripheral tissues. Low-density lipoproteins (LDL) are formed from VLDL and are catabolized primarily by the high affinity of the LDL receptor. Atorvastatin reduces plasma cholesterol and lipoprotein levels, inhibiting HMG-CoA reductase and cholesterol synthesis in the liver and increasing the number of liver LDL receptors on the surface of cells, increasing LDL uptake and catabolism.
Atorvastatin reduces LDL production and the number of LDL particles, it also produces a deep and sustained elevation in LDL receptor activity, as well as a beneficial change in the quality of circulating LDL particles. Atorvastatin effectively reduces LDL in patients with familial homozygous hypercholesterolemia, a population that has not responded adequately to lipid-lowering medication.
In a dose-response study, Atorvastatin reduced C-total (30% – 40%), LDL-C (41% – 61%), apolipoprotein B (34% – 50%), and triglycerides (14% – 33 %), while it produced variable elevations in HDL-C and apolipoprotein A. These results are consistent in patients with family homozygous hypercholesterolemia, unfamily forms of hypercholesterolemia and mixed hyperlipidemia, including patients with non-insulin dependent diabetes mellitus.
Pharmacokinetics and metabolism
Absorption: Atorvastatin is rapidly absorbed after oral administration; their peak plasma concentrations occur within one to two hours. The amount of absorption and plasma concentrations of Atorvastatin rise in proportion to the dose. Atorvastatin tablets are bioavailable between 95% and 99% compared to solutions. The absolute bioavailability of Atorvastatin is approximately 12% and the systemic availability of HMG-CoA reductase inhibitory activity is approximately 30%. The low systemic availability is attributed to presystemic clearance in the gastrointestinal mucosa and / or in the first-pass metabolism of the liver. Although food decreases the frequency and amount of its absorption by approximately 25% and 9% respectively, however, it has been verified by Cmax and ABC that the reduction in LDL-C is similar if Atorvastatin is administered with or without food. . Plasma Atorvastatin concentrations decrease (approximately 30% for Cmax and ABC) after administration of the drug in the evening compared to that in the morning. However, the reduction of LDL-C is the same, regardless of the time of day when the drug is administered.
Distribution: The average volume of distribution of Atorvastatin is approximately 381 liters. Atorvastatin is bound to plasma proteins by> 98%. The red blood cell / plasma ratio of approximately 0.25 indicates poor penetration of the drug into red blood cells.
Excretion: Atorvastatin and its metabolites are mainly eliminated in the bile after hepatic and / or extrahepatic metabolism; however, the drug did not appear to undergo enterohepatic recirculation. The average plasma elimination half-life of Atorvastatin in humans is approximately 14 hours, but the half-life of HMG-CoA reductase inhibitory activity is between 20 and 30 hours due to the contribution of active metabolites. Following oral administration, less than 2% of the Atorvastatin dose is recovered in the urine.
Pharmacodynamics: Atorvastatin and its metabolites are pharmacologically active in humans, its primary site of action is the liver, which is the main site of cholesterol synthesis and LDL clearance. The reduction of LDL-C correlates better with the dose of the drug than with the systemic concentration of the drug. The individualization of the dose of the drug should be based on the therapeutic response.
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/2″]
Indications
Statin is indicated as a diet-associated treatment for the reduction of elevated total cholesterol, LDL cholesterol, apolipoprotein B, and triglycerides in patients with primary hypercholesterolemia, combined (mixed) hyperlipidemia, and homozygous and heterozygous family hypercholesterolemia when responding to diet or other measures. Non-pharmacological are inadequate.
Contraindications
Statin is contraindicated in patients hypersensitive to any component of the product, or who have active liver disease or unexplained persistent elevations of serum transaminases that exceed three times the upper normal limit; also in those patients who are pregnant, lactating or of reproductive age and who are not using adequate contraceptive methods. Statin 10 mg, Statin 20 mg and Statin 40 mg should be administered to women of reproductive age only when they have a high security of contraception or after having been informed of the potential risk to the fetus.
Warnings
Liver Effects: As with other lipid lowering agents of the same class, moderate elevations (> 3 times the upper normal limit [LNS] of serum transaminases have been reported after therapy with Atorvastatin). Those patients who develop any symptoms or signs that suggest liver dysfunction should undergo liver function tests. Patients whose transaminase levels are elevated should be evaluated until this abnormality is resolved. Effects at the musculoskeletal level: Myalgia has been reported in patients treated with Atorvastatin, myopathy, defined as muscle pain or weakness in conjunction with elevations in creatinine phosphokinase (CPK) with values 10 times greater than the upper normal limit. Patients should be alerted to report any unexplained muscle pain, weakness, or tenderness immediately, especially if accompanied by general malaise or fever. Atorvastatin therapy should be discontinued if CPK levels rise markedly, if myopathy is suspected or diagnosed. The risk of a myopathy during treatment with other drugs in this class increases with the co-administration of cyclosporine, fibric acid, erythromycin, niacin or azole antifungals. Specialists considering combination therapy with Atorvastatin and fibric acid derivatives, erythromycin, immunosuppressive drugs, azole antifungals, or niacin lipid-lowering doses, should weigh the potential benefit and risks, as well as carefully evaluate the patient in case signs or symptoms of muscle pain, tenderness or weakness appear, especially during the first months of therapy and during periods of elevation or titration of the doses of any of these drugs. Regular evaluations of creatinine phosphokinase (CPK) should be performed in such situations, but there is no assurance that these evaluations will prevent the occurrence of severe myopathy. Atorvastatin therapy should be temporarily suspended or discontinued if any patient has a serious and acute condition that suggests myopathy or has a risk factor that predisposes them to the development of renal dysfunction secondary to rhabdomyolysis (eg acute and severe infection, hypotension, major surgery, trauma, severe endocrine or electrolyte metabolic disorders and uncontrollable seizures).
[/vc_column][vc_column width=»1/2″ style=»background-color:#f4f4f4; height:100%; padding-left:10px; padding-right:10px;»]
Composition
Statin 10 :
Each coated tablet contains:
Atorvastatin Calcium Trihydrate equiv. at 10 mg.
C.S.P. excipients 1 tablet
Statin 20 :
Each coated tablet contains:
Atorvastatin Calcium Trihydrate equiv. at 20 mg.
C.S.P. excipients 1 tablet
Statin 40 :
Each coated tablet contains:
Atorvastatin Calcium Trihydrate equiv. at 40 mg.
C.S.P. excipients 1 tablet
Posology and administration
The patient must enter an adequate diet to lower cholesterol, prior to the start of treatment with Statin and must continue during treatment. The initial daily dose is 10 mg. Dosing will be done individually according to baseline LDL-C levels, therapy goals, and patient response. Dose adjustments should be made at intervals of four weeks or more. The maximum daily dose should not exceed 80 mg. The dose can be administered at any time of the day, with or without food.
Primary hypercholesterolemia and combined (mixed) hyperlipidemia: Most patients are controlled with 10 mg of Atorvastatin administered once daily. A therapeutic response is evident during the first two weeks of administration, and a maximum response is usually achieved within the first 4 weeks. The response is maintained during chronic therapy.
Family homozygous hypercholesterolemia
Adults: In a study in patients with family homozygous hypercholesterolemia, most patients responded to an 80 mg dose of Atorvastatin with a greater than 15% reduction in LDL-C (18% – 45%).
Children: The experience of treatment in a pediatric population (with doses of up to 80 mg / day of Atorvastatin) is limited.
Dosage in patients with renal impairment: Renal diseases have no influence on plasma concentrations or the reduction of Atorvastatin in LDL-C; therefore, no dose adjustment is required.
Use in geriatrics: The efficacy and safety in elderly patients (over 70 years old) using recommended doses, is similar to that seen in the general population.
Presentation
Statin 10 – box containing 20 coated tablets.
Statin 20- box containing 20 coated tablets.
Statin 40 – box containing 20 coated tablets.
Storage Recommendations
Store below 30 °C. Protect from light and moisture.
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
Cautions
General: Before starting Statin therapy, attempts should be made to control hypercholesterolemia through proper diet, exercise, and weight reduction in obese patients, thereby treating other inherent medical problems. Atorvastatin may cause an elevation in creatinine phosphokinase and transaminase levels.
Information to patients: Patients should be prevented from reporting any unexplained muscle pain, tenderness, or muscle weakness, particularly if accompanied by general discomfort or fever.
Interaction with other drugs: The risk of myopathy during treatment with other drugs of the same class increases, if Atorvastatin is administered together with cyclosporine, fibric acid derivatives, erythromycin, azole antifungals or niacin. Antacids: Co-administration of Atorvastatin with an oral suspension of an antacid containing magnesium and aluminum hydroxide decreases plasma concentrations of Atorvastatin by approximately 35%; however, the reduction of LDL-C remains unchanged.
Antipyrine: Because Atorvastatin does not affect the pharmacokinetics of antipyrine, an interaction with other metabolized drugs of the same cytochromic isozymes is not expected.
Cholestyramine: Plasma concentrations of Atorvastatin and Digoxin raise stable plasma Digoxin concentrations by approximately 20%. Patients who are under treatment with digoxin should be properly evaluated. Erythromycin: In healthy patients, co-administration of erythromycin (500 mg QID), a known cytochrome P450 3A4 inhibitor, is associated with increased plasma concentrations of Atorvastatin.
Oral Contraceptives: Co-administration of oral contraceptives containing norethindrone and ethinyl estradiol raised the ABC values of norethindrone and ethinyl estradiol by approximately 30% and 20% respectively. These elevations should be considered when choosing an oral contraceptive in women who are taking Atorvastatin. Interaction studies of Atorvastatin with warfarin and cimetidine were performed; no significant clinical interactions were reported. Use in pregnancy and lactating mothers: Atorvastatin is contraindicated in pregnancy and during lactation. Women of childbearing age should take adequate contraceptives. Atorvastatin should be administered to women of reproductive age only when conception is unlikely in such patients and they have been informed of the high risk to the fetus.
It is not known whether this drug is excreted in human milk. Due to its high rate of adverse reactions in infants, women receiving Atorvastatin should not breast-feed.
Pediatric use: Experience with treatment with Atorvastatin in a pediatric population is limited to doses of up to 80 mg / day for one year in 8 patients with familial homozygous hypercholesterolemia (FH). No clinical or biochemical abnormalities were reported in these patients.
Side effects
Statin is generally well tolerated. Adverse reactions have generally been mild and transient. The most frequent adverse effects (> 1%) associated with therapy with Atorvastatin, in patients who participated in controlled clinical studies were constipation, flatulence, dyspepsia, abdominal pain, headache, nausea, myalgia, asthenia, diarrhea and insomnia. The following additional side effects were reported in clinical trials with Atorvastatin: muscle cramps, myositis, myopathy, paresthesia, peripheral neuropathy, pancreatitis, hepatitis, cholestatic jaundice, anorexia, vomiting, alopecia, pruritus, rash, impotence, hyperglycemia, and hypoglycemia. Not all of the stated effects have been causally associated with Atorvastatin therapy.
[/vc_column][/vc_row]
