[vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-bottom:0px; padding-bottom:0px;»][vc_column alignment=»left» width=»1/2″]
Bronal
Bronal contains prednisolone, which is a glucocorticoid. Glucocorticoids are adrenocortical steroids, of natural or synthetic origin, that are rapidly absorbed from the gastrointestinal tract.
[/vc_column][vc_column width=»1/2″]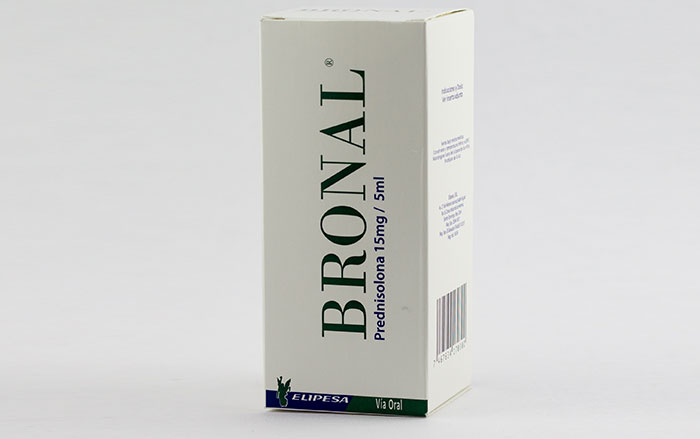 [/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
Clinical Pharmacology
Glucocorticoids of natural origin (hydrocortisone and cortisone) are used as a replacement therapy in states of adrenocortical deficiency. Its synthetic analogues such as prednisolone are primarily used for their powerful anti-inflammatory effects in disorders of many organs. Glucocorticoids such as prednisolone cause varied and profound metabolic effects.
Additionally, they modify the immune response to stimuli. Prednisolone is rapidly and completely absorbed from the gastrointestinal tract after oral administration. It is 70% bound to plasma proteins and is eliminated from plasma with a half-life of 2 to 4 hours. It is mainly metabolized in the liver and excreted in the urine as glucuronide sulfate conjugates. The onset, duration, and maximum effect of action depend on the route / site of administration, the solubility of the pharmaceutical form, the dose administered, the disease to be treated, and the biological half-life.
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/2″]
Indications
In general, prednisolone is the drug of choice for all conditions for which routine systemic corticosteroid therapy is indicated:
Allergic States:
In severe or unresponsive allergies to conventional treatment: perennial or seasonal allergic rhinitis, bronchial asthma, contact dermatitis, atopic dermatitis, drug hypersensitivity reactions, serum diseases.
Dermatological Diseases:
Pemphigus, dermatitis herpetiform, severe erythema multiforme (Stevens Johnson Syndrome), exfoliative dermatitis, mycosis, severe, psoriasis, severe seborrheic dermatitis.
Respiratory diseases:
Symptomatic sarcoidosis, Loeffer’s syndrome unmanageable by other means, berylliosis, pulmonary or fulminant tuberculosis when administered in conjunction with appropriate anti-tuberculosis chemotherapy and aspiration pneumonitis.
Rheumatic Disorders:
As supportive therapy in short-term treatment (to assist the patient in acute episodes or exacerbations) in: Psoriatic arthritis, rheumatoid arthritis including juvenile rheumatoid arthritis (some cases may require low-dose maintenance therapy), ankylosing spondylitis, acute and subacute bursitis, acute gouty arthritis, post-traumatic osteoarthritis, osteoarthritis, epicondylitis.
Collagen Diseases:
During an exacerbation or as maintenance therapy in cases of: systemic lupus erythematosus and acute rheumatic carditis.
Gastrointestinal diseases:
To help the patient in critical periods of the disease: ulcerative colitis and regional enteritis.
[/vc_column][vc_column width=»1/2″ style=»background-color:#f4f4f4; height:100%; padding-left:10px; padding-right:10px;»]
Composición
Bronal Syrup
Prednisolone (as disodium phosphate) 15mg
C.S.P. excipients 5ml
Bronal Coated Tablets:
Bronal – 5
Prednisolone (as disodium phosphate) 5mg
C.S.P. excipients 1 comp.
Bronal – 10
Prednisolone (as disodium phosphate) 10mg
C.S.P. excipients 1 comp.
Bronal – 20
Prednisolone (as disodium phosphate) 20mg
C.S.P. excipients 1 comp.
Administration route
Oral
Presentation
Box containing a bottle with 60ml of syrup with a measuring cup.
Box containing a blister with 10 5mg coated tablets.
Box containing a blister with 10 10mg coated tablets.
Box containing a blister with 10 20mg coated tablets.
Storage Recommendations
Keep in a cool place (below 30 °C). Protect from light and moisture.
Contraindications
Bronal is contraindicated in case of systemic fungal infections.
[/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
Drug Interactions
Prednisolone presents the interactions of glucocorticoids, drugs administered before and during treatment, and which induce the activation of microsomal enzymes at the liver level such as rifampicin, barbiturates and phenytoins, may shorten the elimination half-life of prednisone and prednisolone.
[vc_row_inner style=»margin-top:0px; margin-bottom:0px; padding-top:0px;»][vc_column_inner width=»1/2″]
Prednisolone:
- Decreases action of: Chloramphenicol and cephalosporins.
- Increases blood levels of Theophylline.
- Risk of spread with tuberculostatic agents.
- Increase K elimination with: diuretics.
- Increases toxicity of both with: salicylates.
- Power sedative effect of CNS depressants.
- Less action of:
- Anticholinergics.
- Estrogens.
- Progesterone.
- Testosterone.
- Diphenylhydantoin.
- Griseofulvin.
- Anticholinergics.
- Effect enhanced with:
- Alkalinizers
- Procarbazine.
- Coronary vasodilators with group N.
- Alkalinizers
- Decreased effect with:
- Acidifying.
- β-blockers.
- Betazole.
- Acidifying.
[/vc_column_inner][vc_column_inner width=»1/2″ style=»background-color:#f4f4f4; height:100%; padding-left:10px; padding-right:10px;»]
Side effects
Fluid and sodium retention, potassium loss, hypokalemic alkalosis and hypertension, muscle weakness, osteoporosis, steroid myopathy, peptic ulcer, pancreatitis, ulcerative esophagitis. Fragile skin, petechiae and ecchymosis, facial erythema, increased sweating.
Neurological disorders such as: vertigo, headache. Menstrual irregularities. Development of cushingoid syndrome. Growth suppression in children. Manifestations of latent diabetes mellitus. Glaucoma, exophthalmia, and posterior subcapsular cataracts.
[/vc_column_inner][/vc_row_inner][/vc_column][/vc_row][vc_row inner_container=»true» bg_color=»#ffffff» style=»margin-top:0px; margin-bottom:0px;»][vc_column width=»1/1″]
Posology and Administration
The BRONAL dose should be individualized according to the patient’s response and the severity of the disease. For infants and children the recommended dose should be governed by the same consideration, rather than strict adherence to the range indicated by age or body mass. Hormone therapy is an adjuvant but is not a replacement for conventional therapy. The dose should be gradually decreased or discontinued when the medicine has been administered for several days. The severity, prognosis, expected duration of the disease, and the patient’s chronic reaction to the medication are the primary factors determining the dose. If a spontaneous remission period occurs in a chronic condition, treatment should be discontinued. In the treatment of children with acute severe asthma exacerbations, the recommended dosage ranges from 1 to 3 mg prednisolone / kg / day. The initial dosage should be maintained or adjusted until a satisfactory response is achieved.
The initial dose of BRONAL, in adults, can vary from 5 mg to 60 mg per day depending on the specific disease to be treated. In less serious situations lower doses will suffice, while some patients will require higher doses. The initial dose should be maintained or adjusted until a satisfactory response is achieved. If after a reasonable time there is no clinical response, BRONAL should be discontinued and other therapy initiated.
IT SHOULD BE EMPHASIZED THAT THE DOSAGE REQUIREMENTS ARE VARIABLE AND MUST BE INDIVIDUALIZED ACCORDING TO THE DISEASE UNDER TREATMENT AND THE RESPONSE OF THE PATIENT.
After a favorable response, the appropriate dose should be established and the initial dose gradually decreased with small portions.
Warnings
Corticosteroids can mask some signs of infection and new infections can appear during their use, in addition, prolonged use of them can cause eye disorders.
Use in pregnancy: The use of corticosteroids in pregnant women, lactating women or women with the possibility of becoming pregnant, requires that its benefits be weighed against the potential dangers for the mother and the embryo or fetus. Children born to mothers who have received significant doses of corticosteroids during pregnancy should be carefully observed to treat symptoms of hypoadrenalism. Patients undergoing corticosteroid therapy should not be vaccinated against chickenpox. The use of BRONAL in active tuberculosis should be restricted to those cases of fulminant or disseminated tuberculosis in which the corticosteroid is used for the treatment of the disease together with an adequate anti-tuberculosis regimen.
Cautions
The lowest possible dose of mineralcorticoids should be used to control the condition under treatment and when possible to reduce it; This reduction should be gradual. Psychic disorders can appear when corticosteroids are used, which vary from euphoria, insomnia, variable mood, personality changes and severe depression, to manifestations of frank psychosis. Emotional instability also occurs and psychotic tendencies can worsen. The aspirin-corticosteroid combination should be used with caution in patients with hypothrombinemia.
Corticosteroids should be used with caution in patients with non-specific ulcerative colitis, as there may be a likelihood of imminent perforation, abscesses or other pyogenic infections, diverticulitis, recent intestinal anastomosis, latent active peptic ulcer, kidney failure, hypertension, osteoporosis, and myasthenia gravis.
The growth and development of infants and children receiving prolonged corticosteroid therapy should be carefully observed.
Pediatric use
In the treatment of endocrine disorders, such as primary and secondary adrenocortical insufficiency in childhood, mineralcorticoid supplementation is of particular importance. Children born to mothers who have received considerable doses of corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Immunization procedures should not be taken by patients who are on corticosteroid therapy. Pediatric patients who take medications that suppress the immune system are more susceptible to infections than healthy pediatric patients.
In non-immune patients with corticosteroid treatment, chicken pox and measles, for example, can have a severe or fatal course. Growth and development in children receiving prolonged corticosteroid therapy should be carefully observed.
[/vc_column][/vc_row]
